Background: In 2017, hydroxyurea was approved for the treatment of all sickle cell patients with genotype HbSS in Uganda following overwhelming support from the NOHARM trial conducted in a malaria endemic region at Mulago National Referral Hospital's Sickle Cell Clinic. Between January 2019 and June 2022, immediately following nationwide approval and distribution of hydroxyurea, hydroxyurea was prescribed a total of 4017 (51.2%) times out of the 7851 HbSS patient visits to the clinic according to data available from the clinic.
Aims:The purpose of this study is to investigate the knowledge, perceptions, and beliefs of patients with sickle cell disease and their caregivers attending this clinic in Kampala regarding their disease, complications, genetic impact, general anticipated course of treatment or natural history of disease, and hydroxyurea.
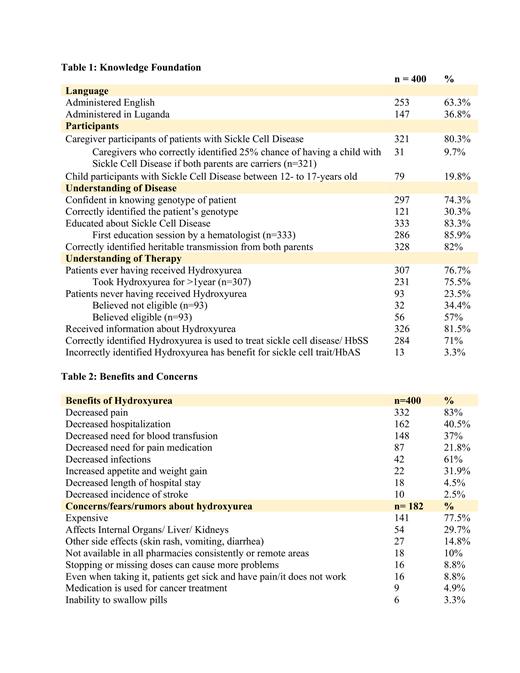
Methods: A total of 400 (56%) out of 713 patients were surveyed over a 3-week period using standardized, pretested questionnaires administered orally by trained research personnel in both English (253, 63%) and Luganda (147, 36.8%), which are the most common local languages and dialects spoken by patients in Kampala. Three-hundred and twenty-one (80.3%) participants were caregivers and 79 (19.8%) were children with sickle cell disease between 12- and 17-years-old.
Results: Most participants reported receiving counseling about sickle cell disease (333; 83.3%) largely by hematologists (286; 85.9%), however, several knowledge gaps were identified. Two-hundred and ninety-seven (74.3%) participants reported not knowing the type of sickle cell or genotype of the patient. Moreover, presentation of various options did not significantly improve recognition of the correct genotype, with only 121 (30.3%) participants correctly identifying HbSS. Three-hundred and twenty-eight (82%) participants correctly identified the heritable transmission of the disease from both parents; however, caregivers exhibited limited understanding of genetic risk with only 31 (9.7%) correctly identifying the one in four chances of having a subsequent child with sickle cell disease when both parents are carriers.
Hydroxyurea counseling was reported by 326 (81.5%) of participants, and 307 (76.7%) participants reported that the patient received hydroxyurea, with most patients taking the medication for at least 1 year. Of the 93 (23.5%) participants who identified the patient had never received hydroxyurea, 32 (34.4%) were uncertain if the patient would be eligible and 56 (57%) believed the patient was eligible to take the medication. Participants identified hydroxyurea benefits as decreases in pain (332; 83%), hospitalization (162; 40.8%), need for blood transfusion (148; 37%), need for pain medication (87; 21.8%), infections (42; 61%), weight loss (22; 31.9%), length of hospital stay (18; 4.5%), and incidence of stroke (10; 2.5%).
Slightly more than half of patients had no concerns about hydroxyurea (218; 54.5%). Most patients with concerns (182; 45.5%) identified hydroxyurea's high cost as their main concern (141; 77.5%). Other rumors and fears about hydroxyurea included: negative affects on internal organs such as the liver or kidneys (54; 29.7%), other negative side effects (27; 14.8%), inaccessibility in pharmacies and remote areas (18; 10%), harm due to stopping or missing doses (16; 8.8%), ineffectiveness (16; 8.8%), additional indications as a cancer medication (9; 4.9%), and younger children's difficulty swallowing pills (6; 3.3%).
Conclusion:Given the significantly improved morbidity and mortality of sickle cell patients who are adherent to hydroxyurea, it is necessary to address the rumors, misconceptions, and gaps in understanding of the genetic impact of the disease as well as the risks and benefits of hydroxyurea therapy. At the population level, learning is impacted by education levels, literacy rates, health literacy rates, and other cultural and societal factors, thus teaching should be culturally competent and inclusive with verbal and visual methods. The high cost of the medication and lack of consistent supply seem to be the most prohibitive factors in patient acceptance and adherence to take hydroxyurea. With only 1% of Uganda's population covered by health insurance, it is imperative for system-wide changes to address the affordability and accessibility of hydroxyurea and/or to extend the coverage of health insurance to those in need.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal